Rewired: Jazmine Bonner's VNS Journey After Stroke at Age 35
May 2, 2025
By: WakeMed Rehab & Physical Therapy
Categories: Raleigh Campus, Stories, Foundation, Emergency, Physical Therapy, Women's
Jazmine Bonner was a typical 35-year-old mom of one. Very proud of her football player son, she relished her after-work hours spent cheering him on and providing a fun-filled life. One day in September 2023 after arriving home from one of her son's games, their predictable and comfortable lifestyle was suddenly upended.
"My body started to cramp up and stiffen badly," recalls Jazmine. "I was worried about going to the bathroom because I had stopped to pick up dinner and had been holding it, so I had to go urgently, but I couldn't get out of the car."
A Sudden Body Constriction
Frantic, Jazmine opened the door and yelled for help to alert both her son inside the apartment as well as a neighbor passing by while walking her dog. The neighbor noticed Jazmine's distress, and ran over to assist. Unable to help Jazmine free herself from the car, the neighbor immediately called 911.
"My son had come home earlier than I had, and he was already in the apartment napping following his game. I am thankful the neighbor heard me and came to my rescue."
EMS to the Rescue
Within minutes, emergency medical services (EMS) arrived and began asking Jazmine questions. The first responders took note of her slurred speech and left-side weakness. Loading her onto a stretcher, they notified the WakeMed Raleigh Campus Emergency Department they were bringing in a patient displaying symptoms of a stroke.
Meanwhile, awakened by all the commotion, Jazmine's son went outside and contacted their cousin of his mom's medical emergency, so they could head to the hospital.
Upon arrival to WakeMed Raleigh Campus Emergency Department, Jazmine was taken to imaging for an X-ray as well as computed tomography (CT) scan. She was diagnosed with an ischemic stroke and brain swelling. She also continued to show pronounced issues with slurred speech and left-side paralysis.
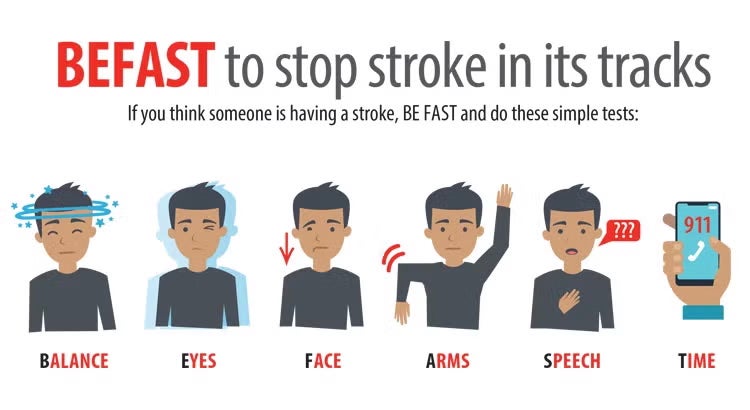
Symptom Knowledge is Power: BEFAST!
"I was fighting the EMS workers and doctors regarding the diagnosis. I thought someone who had a stroke would smell burnt toast, and I didn't have that symptom, so I figured they had it wrong. They educated me about BEFAST symptoms of stroke."
Surgery to Support Brain Recovery
"Swollen blood vessels had caused my brain to swell, so neurosurgeon Lars Benjamin Gardner, DO, performed a craniotomy to relieve the pressure on my brain. Thereafter, I remained at WakeMed with round-the-clock care for the next six months."
In November 2023, Jazmine was strong enough to transfer from the Raleigh Campus E tower to WakeMed Rehabilitation Hospital. She received speech, occupational, recreational and physical therapy from several therapists, with a focus on strengthening her ability to utilize her left side and recover her speech and cognitive function.
By February 2024, Jazmine was discharged home into the care of a loved one. She had to give up her apartment and quit her job, but she was grateful to be alive and to walk with only a cane.
Of that season in her life, Jazmine shares, "It was terrible, but I'm grateful for everyone at WakeMed. They were all really supportive."
WakeMed Stroke VNS Rehab
Because of her upper limb impairment due to her stroke, Jazmine was unable to return to work, and had to go on disability. Yet, hope was on the horizon. In November 2024, she learned about WakeMed’s Stroke VNS Rehabilitation. Within WakeMed’s Stroke Program, neurosurgeons, neurologists and occupational therapists collaborate to offer vagus nerve stimulation (VNS) via a safe and small implanted FDA-approved device to improve hand and arm mobility for ischemic stroke survivors.
When used in combination with outpatient occupational therapy and at-home activities, this breakthrough treatment activates the parts of the brain (via the vagus nerve) that are important for motor learning and generates two to three times more hand and arm function for stroke survivors than active rehabilitation therapy, even years later.
On December 31, 2024, as a welcome entry into the new year, Jazmine underwent the procedure to place the VNS implant device under the skin in the upper left chest wall and neck region. This same-day, outpatient procedure was performed by neurosurgeon Robert Dallapiazza, MD.
From January through March 2025, Jazmine returned to WakeMed for stroke VNS rehabilitation with Amber Lewis, MHA/MSL, OTR/L, CBIS, CSRS, and Kelly Draucker, OTD, OTR/L for three 90-minute occupational therapy sessions per week, for six weeks. Following those 18 visits, Jazmine transitioned to therapy twice per week for 45-minute sessions for three more weeks.
During the sessions, the therapist uses a remote that sends a wireless signal to the implanted device to deliver a brief, gentle pulse to the vagus nerve while Jazmine performs various therapy tasks.

Draucker explains, "The goal of stroke VNS therapy is to help stroke survivors recover more of their upper extremity function so they can get back to doing the things that matter most to them. Whether it’s going back to work, being active again with hobbies, or doing household work, it’s important that we help patients identify their goals before therapy so that we can work together to design task-specific sessions that will help improve their hand and arm functions."
In therapy, different interventions and technology are incorporated to problem-solve the environment at home and to provide tools for consistent usage of the arm and hand at home.
Draucker notes, "Jazmine has been most impacted by her ability to put her left arm around her son to give him a hug. Those kinds of functional methods to integrate her left arm are so impactful. Some of the therapies used in session include the Saebo glove, electrical stimulation, reaching tasks, grasping and pinching to aid in her ability to open and close a door, turn pages in a book, open a drawer, lift her arm to apply deodorant with her other arm and so much more to help her gain a wider understanding of how to use her arm."
Jazmine's Life Today

At home, Jazmine is able to self-activate VNS therapy by swiping a magnet across her implant. Each magnet swipe delivers 30 minutes of VNS while Jazmine performs activities of daily living, including shopping, cooking, exercising and more.
"I hope it will help me depend on my left side more instead of just my right. I would love to return to work," says Jazmine.
About WakeMed Physical Therapy
It’s our goal at WakeMed Physician Practices – Physical Therapy to get you back to your active lifestyle. Our techniques are based on national best practices to ensure you receive the latest, best treatment for your condition. We provide physical therapy and occupational therapy in Raleigh, Cary, the Brier Creek area and Apex, North Carolina.
About WakeMed Outpatient Neuro Rehabilitation
At WakeMed Outpatient Neuro Rehabilitation, our physical therapists, occupational therapists, and speech therapists excel in evaluating and treating adults and older children after stroke, spinal cord injury, traumatic brain injury, concussion, and other neurological conditions. Our practices in Raleigh, Cary and Clayton are staffed by specialty trained, passionate therapists who work one-on-one with clients to help them achieve their goals.
About the WakeMed Stroke Program
Our Stroke Program is distinct in providing a comprehensive approach, moving from prevention to management. Our dedicated team of specialists, renowned for their expertise, use physical medicine and rehabilitative techniques at strategic steps along the route to recovery to support the best outcomes. Here are just a few of our impressive features as a thrombectomy-capable stroke center:
- Collaboration with EMS providers to facilitate rapid assessment and transport to the hospital
- Team approach that helps minimize time from arrival to administration of thrombolytics
- Availability of neuroradiologists for quick, expert interpretation of imaging
- Neurology and neurosurgery coverage 24 hours a day, seven days a week for evaluation and treatment
- Neuro intensive care unit for optimization of care for patients with severe strokes
- Nursing staff skilled in assessment and care of stroke patients
- Designated nursing unit for the care of patients with neurological and neurosurgical diagnoses
- Interdisciplinary care planning involving physicians, nurses, case managers, therapists and other services, such as nutritionist consultation and pastoral care
- Comprehensive post-discharge rehabilitation services, including specialty services, such as vestibular rehab to treat dizziness and vertigo
- Public education and awareness programs that focus on risk factor reduction for stroke prevention
- A variety of stroke support groups at several locations throughout North Carolina.
About Kelly Draucker, OT, OTR/L
 Kelly Draucker is an occupational therapist who enjoys treating complex patients with neurological issues related to spinal cord injury, traumatic brain injury and stroke. She also helps patients who have had upper extremity amputations regain independence and the ability to do daily activities with and without a prosthesis.
Kelly Draucker is an occupational therapist who enjoys treating complex patients with neurological issues related to spinal cord injury, traumatic brain injury and stroke. She also helps patients who have had upper extremity amputations regain independence and the ability to do daily activities with and without a prosthesis.
Draucker completed her bachelor’s and doctorate degrees in occupational therapy at Creighton University. Improving a patient’s quality of life is the reason she chose occupational therapy as her general career path. She finds working with patients who are recovering from neurological injuries and illnesses tremendously rewarding because of the dramatic progress that is possible.
About Amber Lewis, MHA/MSL, OTR/L, CBIS, CSRS
 Amber Lewis is an occupational therapist who specializes in restoring function for patients recovering from various neurological conditions including but not limited to stroke, traumatic brain injury, spinal cord injury and multiple sclerosis. She treats patients on land and in the water with specialization in Neuroaquatics. Lewis has a love for learning and technology. She earned her bachelor’s degree in occupational therapy from Winston-Salem State University and dual master’s degrees in administration and leadership from Pfeiffer University. She is also a certified Brain Injury Specialist and certified Stroke Rehabilitation specialist. Lewis is trained in neurodevelopmental treatment (NDT) and Neuro-IFRAH®, whole-person rehab approach. Rehab technology can significantly benefit a patient’s recovery and ability to adapt to new ways of doing things. Lewis is a Level II Saebo clinician and is highly experienced in additional therapeutic technologies such as the Bioness H200, the Bioness Integrated Rehab System, InMotion robotic arms and the Touch bionic-robotic hand.
Amber Lewis is an occupational therapist who specializes in restoring function for patients recovering from various neurological conditions including but not limited to stroke, traumatic brain injury, spinal cord injury and multiple sclerosis. She treats patients on land and in the water with specialization in Neuroaquatics. Lewis has a love for learning and technology. She earned her bachelor’s degree in occupational therapy from Winston-Salem State University and dual master’s degrees in administration and leadership from Pfeiffer University. She is also a certified Brain Injury Specialist and certified Stroke Rehabilitation specialist. Lewis is trained in neurodevelopmental treatment (NDT) and Neuro-IFRAH®, whole-person rehab approach. Rehab technology can significantly benefit a patient’s recovery and ability to adapt to new ways of doing things. Lewis is a Level II Saebo clinician and is highly experienced in additional therapeutic technologies such as the Bioness H200, the Bioness Integrated Rehab System, InMotion robotic arms and the Touch bionic-robotic hand.
Lewis loves being a part of someone’s recovery journey and helping them regain their independence and function. Occupational therapy allows her to creatively blend science, technology and human connection to change a person’s brain and their life. In her spare time, Lewis enjoys travel and laughing with friends and family.
About Robert Dallapiazza, MD, PhD
 Dr. Dallapiazza joined Raleigh Neurosurgical Clinic in 2022 to start up and lead the functional neurosurgery program at RNC and WakeMed. He focuses on stereotactic, functional, and general neurosurgery. He’s also trained in deep brain stimulation (DBS), a procedure that treats movement disorders through electrodes implanted in the brain.
Dr. Dallapiazza joined Raleigh Neurosurgical Clinic in 2022 to start up and lead the functional neurosurgery program at RNC and WakeMed. He focuses on stereotactic, functional, and general neurosurgery. He’s also trained in deep brain stimulation (DBS), a procedure that treats movement disorders through electrodes implanted in the brain.
Dr. Dallapiazza earned his medical degree and doctoral degree in pharmacology through the Medical Scientist Training Program at the University of Iowa Carver College of Medicine. He followed that with a residency in neurosurgery at the University of Virginia School of Medicine, where he served as chief resident, and a fellowship in stereotactic and functional neurosurgery at Toronto Western Hospital in Toronto, Ontario.
He is board certified by the American Board of Neurological Surgery.
Dr. Dallapiazza has authored numerous peer-reviewed publications and contributed to several books, most recently Operative Techniques in Epilepsy Surgery. In 2021, he was named a Best Doctor by New Orleans Magazine.