TAVR
When you need a new heart valve but you are not a candidate for surgery Transcatheter Aortic Valve Replacement (TAVR) might be for you.
Approximately 7 percent of Americans age 65 and older have aortic valve disease. It is likely 50 percent of these people will not survive beyond two years after the onset of symptoms, which can include chest pain and/ or tightness, heart palpitations, shortness of breath (especially with exertion) and fatigue. Advanced age, severe aortic valve disease symptoms and symptoms from other health conditions can even completely incapacitate people, eliminating quality of life. These patients are often too sick or too weak to undergo open surgery to replace their diseased valve – the preferred treatment. TAVR can be an option for these types of patients.
At WakeMed interventional cardiologist a cardiothoracic surgeon, and a large team of heart failure specialists, midlevels, nurses, physical therapists, anesthesiologists and radiologists join forces to perform TAVR procedures.
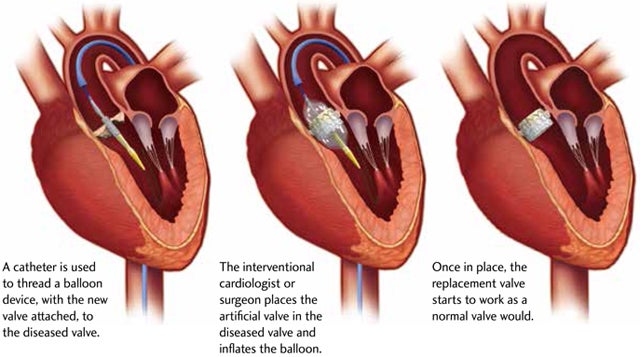
During a TAVR procedure, a very small incision is made in the groin to access the femoral artery or the chest (transapical approach). The cardiologist uses catheters and wires to place the balloon-expandable valve across the old diseased native valve, with the heart still beating. Crimped to the balloon device is the collapsed replacement valve. The surgeon then deploys the new valve within the diseased valve by expanding the balloon together with the new valve. He then secures it into place inside the old valve, displacing the old valve out of the way. In addition, the new valve starts to work as a normal valve should as soon as the balloon is deflated. Most of the time, the patients feel immediately better and start to see improvements in quality of life within several weeks.