What’s the Skinny? Weight Loss Drugs & Your Heart
February 6, 2026
Weight loss drugs have taken the world by storm – making them a hot topic of conversation in and outside of the doctor’s office. Also known as GLP-1 medications, these popular drugs were initially approved to treat type 2 diabetes, but doctors quickly discovered that they also facilitated significant weight loss – thus, the birth of the weight-loss drug craze.
Today, in addition to treating diabetes and obesity, these medications are showing promise in the treatment of countless other health problems, including sleep apnea, kidney disease, inflammation and heart disease. With so much talk, we connected with our experts to shed some light on the latest research and how these drugs affect heart health.
What exactly is a GLP-1?
GLP-1 agonists are a class of medications that mimic hormones in the body to help regulate blood sugar and appetite. Common GLP-1s include liraglutide, semaglutide and tirzepatide – and each is sold and marketed under a variety of other brand names, depending on their dosage and reason for use.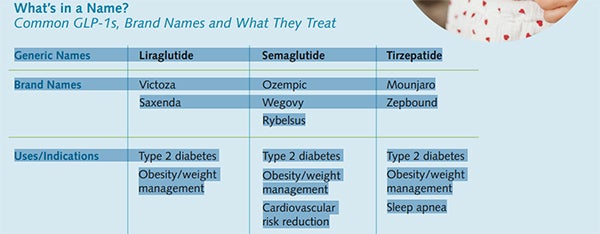
How GLP-1s Could Help the Heart
These medications are primarily used to treat conditions, such as diabetes and obesity, both of which are cardiovascular risk factors. Because diabetes can damage blood vessels, cause high blood pressure and increase the risk for heart attack and heart failure, improving blood sugar can help prevent all of these downstream effects. Similarly, losing weight can lead to improvements in blood pressure, cholesterol and sleep apnea.
New research is also giving us a clearer understanding of how GLP-1s could affect cardiovascular outcomes in specific populations, such as those with known heart disease or certain types of heart failure.
Top Research Studies on GLP-1s and Cardiovascular Outcomes
The November 2023 issue of The New England Journal of Medicine shared results from a research study (SELECT) involving 17,000 patients that showed the use of semaglutide was linked to a 20% reduction in the risk of major adverse cardiovascular events – such as heart disease, stroke and peripheral arterial disease – in patients who had previously been diagnosed with heart disease. In the same study, semaglutide decreased heart failure and all-cause mortality by 18% and 19% (respectively).
The FDA responded to this study by approving Wegovy in March 2024 to reduce the risk of cardiovascular death, heart attack and stroke in adults with cardiovascular disease and either obesity or overweight.
An August 2023 article in The New England Journal of Medicine shared the results of a trial following 529 patients who had heart failure with preserved ejection fraction and obesity. Study results showed that those treated with semaglutide (vs placebo) experienced reductions in symptoms and physical limitations, greater improvements in exercise function and greater weight loss.
In a November 2024 article featured in The New England Journal of Medicine, researchers found that tirzepatide reduced the risk of cardiovascular death or worsening heart failure in patients with heart failure with preserved ejection fraction and obesity.
The study followed 731 patients to track cardiovascular outcomes for patients given tirzepatide or a placebo.
The Bottom Line – Who Needs a GLP-1?
Based on current guidelines, if you don’t have type 2 diabetes or obesity, you may not benefit from or qualify for taking a GLP-1. If you’re interested in learning more, your primary care doctor is the best place to start the discussion.
In most cases, GLP-1 medications are used to treat obesity and diabetes – both of which are managed in primary care. At the same time, cardiologists are closely following the research and exploring treatment for certain populations.
“While this cardiovascular data is certainly promising, prescribing GLP-1s in cardiology has not yet become mainstream – there’s still so much to learn and the data is coming in quickly,” explains Dr. Raj Fofaria, WakeMed Heart & Vascular – Cardiology. “We are, however, starting to talk with very select groups of patients who we think may benefit from taking them – particularly in our Advanced Heart Failure practice. There’s significant data to support that heart failure patients could see improved symptoms and quality of life as well as reduce their risk of hospitalization.”
Dr. Fofaria reiterates that every patient’s circumstances are unique, and that all questions around GLP-1s are welcome.
“As with any emerging treatment, we know our patients have questions. There are few medications that have this widespread use or consumer awareness, and we want our patients to be informed about both the potential benefits and risks.”
What Else Should We Know about GLP-1s?
WakeMed Clinical Pharmacist Janna Beavers offers the following guidance for evaluating GLP-1 treatment for any indication.
Side effects will vary, but the most common are gastrointestinal in nature (e.g. nausea, diarrhea, vomiting, constipation, bloating). More serious side effects include pancreatitis, gallbladder problems and a rare risk of thyroid tumors.
Monitoring is key. These medications require close monitoring and routine dose adjustments, making it important to stay in touch with your prescribing provider. While there are many third-party websites that offer “discount” GLP-1s, nothing can replace working with a provider who knows you and understands your medical history.
Cost is a common barrier, as most insurance companies do not cover these medications. Even for those with insurance coverage, obtaining approval can take weeks or months, and out-of-pocket costs may exceed $500 a month.
Losing muscle mass is a real concern with these medications, so they should be used in conjunction with a healthy diet and exercise plan. Incorporating a strict strength training routine is particularly important for patients with heart disease.
Janna Beavers shares, “Whether for weight loss, diabetes, sleep apnea or another emerging indication, there are a lot of reasons a provider may recommend a GLP-1 medication. It’s an exciting time for us to see how these medications could transform our practice and WakeMed is eager to remain on the forefront of the field.”