Resilience in the Face of Adversity: How Andrei Lee Channels Military Discipline to Overcome Traumatic Brain Injury
June 23, 2025-(1).gif)
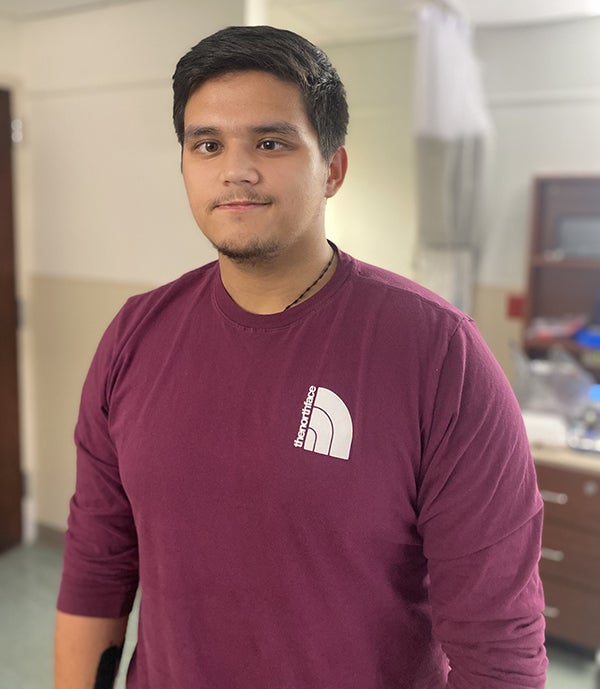
Andrei with nystagmus
Being in the military is an incredible journey that transforms individuals in profound ways. From the moment recruits don their uniforms, they embark on a path filled with rigorous training, camaraderie and self-discovery. Each early morning run and late-night drill sharpens their discipline and resilience, fostering a deep sense of purpose and belonging. The bonds formed with fellow service members become unbreakable, as they share challenges and triumphs in pursuit of a common mission. This unique experience instills values of honor, commitment and sacrifice that last a lifetime. For 21-year-old Andrei Lee, an infantryman currently stationed at Fort Bragg in the United States Army for the last two years, these values rang true.
The Call to Save a Soldier
On May 3, while traveling along Interstate 40 in Raleigh, just a few miles ahead of his fellow Army comrades, Andrei was suddenly sideswiped by another vehicle. The impact sent his car crashing into the highway guardrail, leaving him trapped inside. Thinking quickly, he called his Army buddies and his squad leader, Staff Sergeant Walle, to explain the situation and ask for help. Without hesitation, they rushed to his location. As he waited with his hazard lights flashing, a large box truck barreled into his stalled vehicle at full speed — estimated between 65 and 70 miles per hour.
Upon his squad's arrival on the scene, they saw Andrei in a critical state. Staff Sergeant Walle called 911 and immediately began to administer CPR.
WakeMed Level 1 Trauma Center Team Deploys Into Action
Soon, emergency medical services (EMS) arrived on the scene, loaded Andrei on a gurney and sped him to the WakeMed Raleigh Campus Emergency Department Level 1 Trauma Center.
Andrei received high-quality assessment and care led by general and bariatric surgeon Michael Williford, MD, FACS, Christine Cisek, PA, and other members of the trauma team, including an emergency department physician, neurosurgeon and ear, nose and throat (ENT) consultant. They evaluated Andrei, addressed his life-threatening injuries and put him on the course to healing.
Care from the First Family
Andrei's parents who lived abroad in the Philippines were alerted of his condition along with his siblings who lived in Arizona. Within the hour, his older sister was on her way to WakeMed to be with Andrei for the duration of his hospitalization.
Andrei underwent X-rays and magnetic resonance imaging (MRI) that revealed he'd suffered multiple skull fractures as well as a traumatic brain injury.

Andrei's sister shares, "It was shocking to learn he'd been in an accident. It was 3:00 in the morning when I found out, and I came right away. Our parents were able to make the international flight by the time Andrei was stabilized. Andrei was heavily sedated for two weeks, yet when my parents arrived, he in his drowsy state, made efforts to comfort our parents and assure them silently that he would be okay."
A Steady March Toward Recovery at WakeMed Rehabilitation Hospital
After two weeks, Andrei was fully awakened with medical stability established and pain levels under control enough that he could be transferred to WakeMed's Rehabilitation Hospital. There he received high intensity physical, occupational and speech therapy six days per week until his discharge on June 6 — 16 days later. The team determined he had benign paroxysmal positional vertigo (BPPV) and nystagmus. His BPPV resulted from dislodged calcium carbonate crystals in his inner ear, which provided incorrect messages to the inner ear about movement, leading to impaired balance. Additionally, when patients have BPPV, certain head positions cause nystagmus — an uncontrollable eye movement made up of a fast phase followed by a slow phase of movement. BPPV is treatable by physical therapists specializing in vestibular rehabilitation+.
"My therapy team included Becky Marciszewski and Blair Hobble along with other capable people. Hobble would turn my head to shift crystals that were causing my vertigo. With their help, I was able to walk, move my right arm, stand without falling, feed myself and function again. This radical change happened in just three days of therapy. I think I made such a swift recovery because I went into the therapy willing to do whatever I was asked. Military basic training disciplined me to understand the importance of following instructions without resistance. Plus, it was easy to do as asked in therapy because everyone was so compassionate and caring."
Hobble adds, "I think Andrei’s success is attributable to several factors, including Andrei’s tenacity, his family’s unwavering support and a team of health care providers going above and beyond to achieve the best possible outcome. I’m the vestibular physical therapist who treated Andrei’s BPPV, and although that treatment had a significant impact on his functional status, a handful of things had to happen before I even saw him. First, his primary physical therapist, Becky Marciszewski realized Andrei was at a high risk for BPPV. Additionally, his physician assistant, Shannon Schweitzer, reached out to the Ear, Nose & Throat (ENT) – Head & Neck Surgery team for clearance to do this assessment in light of his skull fractures. Schweitzer understood the poor outcomes associated with untreated BPPV and followed up with clearance for us to do this assessment. I can’t tell you how many times I reviewed videos of Andrei’s nystagmus with my fellow vestibular physical therapist, Sam Ferraro, to make sure I wasn’t missing anything. I collaborated with his occupational therapist to ensure I could do repositioning maneuvers without hurting his shoulder. There’s so much collaboration constantly going on in the background — brainstorming, anticipating needs, asking questions, pooling resources. That’s what makes WakeMed Rehabilitation Hospital so unique."
Andrei also credits his speech therapist, Haley Root, with extending care that allowed for a speedy recovery.
"The speech therapist gave me specific ways to move my face every morning to allow the muscles to come back to feeling again. I could barely move the right side of my face, and now it is mostly back to normal."
A Soldier for Life Hopes to Return to His Calling
Thanks to the incredibly comprehensive, exceptional care received at WakeMed, Andrei has been able to return to military rehabilitation in Fayetteville where it will be determined if he can return to his prior work as an infantryman.
"I'm determined to get back. My staff sergeant suffered two traumatic brain injuries, so that encourages me. If he can do, I can do it."
About the WakeMed Level 1 Trauma Center
About the WakeMed Trauma Program
From pre-hospital and emergency care to surgery, intensive care and rehabilitation, WakeMed’s Trauma program features a network of care and specialists who are dedicated to preserving life and getting patients on the road to recovery. A continuum of services support trauma patients, starting with EMS and our trauma surgeons to spiritual care, imaging, lab, neurosurgeons, orthopaedists, rehab specialists and more.
WakeMed Trauma Centers
As Wake County’s only provider of trauma services and a regional trauma referral center, our two trauma centers — a Level I Trauma Center at Raleigh Campus and a Level III Trauma Center at Cary Hospital — and the WakeMed Trauma teams are standing ready to provide immediate care for the seriously injured.
WakeMed Rehabilitation Hospital
The WakeMed Rehabilitation Hospital is a 73-bed, nationally ranked, specialty program and CARF-accredited rehabilitation hospital in Raleigh, NC, offering inpatient rehab for adults and children. We offer specialty rehab programming for spinal cord injury, brain injury, stroke, limb loss and pediatric patients. Our team consists of highly experienced therapists who specialize in treating the most complex patients. With the positive support of our team of physical therapists, occupational therapists, speech-language pathologists, neuropsychologists, nurses, case managers and physicians, our patients work hard to achieve the best possible outcomes and return to their lives.
WakeMed offers a full continuum of physical rehabilitation services from the acute care settings in all three hospitals, through inpatient rehab in the CARF-accredited Rehabilitation Hospital, to multi-disciplinary outpatient rehabilitation and home health.
