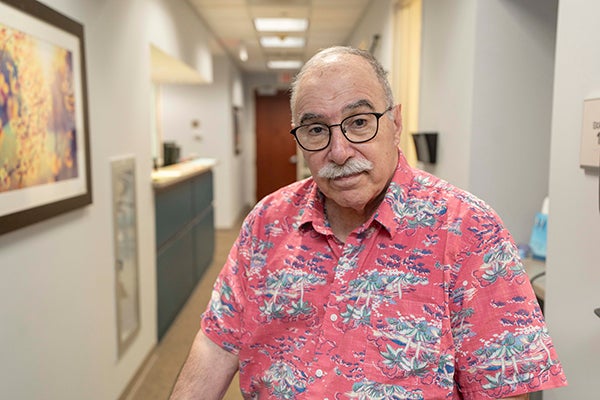
How Lee Asadoorian’s 53rd Wedding Anniversary went from a Heart-Stopping Crisis to Healing Inspiration
October 27, 2025
Categories: Heart & Vascular, Stories, Foundation
Tags: ventricular tachycardia
On September 11, 2024, Lee Asadoorian and his wife, Jane, awoke to celebrate 53 years of marriage. Little did they know, they were in for quite a surprise.
Lee laughs reflecting on that day, "I guess you can say I really know how to treat a lady."
At 8:16 that morning, Lee felt a sudden wave of heat come over his body, followed by a sharp jolt in his chest.
Ventricular Tachycardia Explained
He'd been diagnosed with ventricular tachycardia months prior on June 12. Ventricular tachycardia is a form of arrhythmia, which is an irregular heartbeat. It originates in the heart's lower chambers — ventricles. A normal heart beats between 60 and 100 times per minute when at rest. However, during ventricular tachycardia, the heart rate increases, often exceeding 100 beats per minute. At times, this quickened heartbeat can prevent the heart chambers from adequately filling with blood. As a result, the heart might struggle to pump sufficient blood throughout the body.
A Swift Ride to WakeMed Heart Center
Recognizing the symptoms, Lee urged his wife to call 911.
"By the time emergency medical technicians arrived, I'd had a third one. I had two more in the time it took them to load me into the ambulance."
The emergency medical team informed Lee and Jane that it would be best to take him to WakeMed Raleigh Campus for the state-of-the-art care available at the WakeMed Heart Center, so he endured the ride, eager for medical care.
"I had several more shocks on the way. As I was transitioned to a patient bed, I had the 18th jolt. They immediately started a lidocaine drip, and the heart shocks abruptly stopped. I felt great after that."
A History of Heart Care
Lee has a history of heart issues that began before his episodic ventricular tachycardia. In early 2008, he was diagnosed with atrial fibrillation and received a defibrillator in April 2008. He has been with WakeMed Heart & Vascular in the care of cardiologist Tapan Godiwala, MD, RPVI, since that time. He has also received primary care from Susheel Atree, MD, for over a decade.
Fast Forward to an Anniversary Spent in the Hospital
"I have always been very happy with my provider experiences at WakeMed, so when I was introduced to brand new WakeMed electrophysiologist Neel Patel, DO, I was very assured that I would receive the best care."
Dr. Patel reviewed Lee's chart and informed him that he would perform a ventricular tachycardia ablation on September 13.
"He was a great doctor from the onset. He informed me that I was his first patient at WakeMed, and that he'd done the procedure previously at University of Pennsylvania Hospital. I got excited because that meant he was a hockey Philadelphia Flyers fan. To my surprise, he replied, 'Well, no, I'm from North Jersey, so I'm a New York Rangers fan.' I teased that in that case I'd need a new doctor, and we both had a good laugh."
Ventricular Tachycardia Ablation to the Rescue
The ablation took four hours for Dr. Patel to completely address the ventricular tachycardia inside Lee's heart. Ventricular tachycardia ablation is minimally invasive, using either heat or cold energy to form scars in the heart. This process effectively blocks the abnormal electrical signals responsible for rapid heartbeats. Dr. Patel also performed WakeMed's very first epicardial co2 ablation on top of the heart. This involved going through and opening Lee's chest to stop the tachycardia. Epicardial tachycardia ablation is also a minimally invasive technique aimed at addressing irregular heart rhythms, especially supraventricular tachycardia. The process utilizes radiofrequency energy to form scars in the heart tissue, which interrupt the electrical signals responsible for the fast heartbeats. This procedure is usually carried out when medications do not effectively control the arrhythmia and is regarded as a final option for patients suffering from persistent ventricular tachycardia.
After surgery, Lee awoke feeling great. Dr. Patel informed him that his heart was beating smoothly on its own with no lidocaine.
"I felt amazing, Lee reflects. "In fact, after I awoke, Dr. Patel looked at me and said my heart was pumping well on its own and the tachycardia has been completely resolved."

An Introduction to WakeMed Rehab
With optimal vital signs, on September 15, Lee was discharged home.
"I felt wonderful and had decided to return to the gym when I received a pamphlet in the mail from Dr. Patel on WakeMed Cardiac Rehab. I decided to join and sent in my information. The rehab team called and informed me that because my heart was in such great shape, they were going to sign me up for Pulmonary Rehab and Cardiopulmonary Therapy – Raleigh instead. This program is a bit more strenuous."
In early January 2025, Lee started the program. Cardiopulmonary therapy is available to patients with breathing problems. Patients who benefit from therapy before or after a surgical procedure of any kind or who need to rebuild their breathing endurance are welcome to the WakeMed program.
"I'm glad I did cardiopulmonary rehab. It was very active. The reason was my ejection fraction, the amount of blood my heart pumps out, is much more than what therapists would see in cardiac rehab, so I was in better shape than many other heart patients and got to enjoy the more rigorous program."
Lee's Life Today
Following rehab, Lee met with Dr. Patel and asked if he was cleared to return to the gym for strength training.
"Dr. Patel said absolutely, and I started going three days a week, alternating my focus between the lower and upper body with each visit. I feel strong and very healthy today."

Since recovering, along with going to the gym, Lee and Jane spend their time enjoying neighborhood walks and watching murder mystery television shows.
In considering how wonderful he feels today, Lees exclaims, "I can't say enough good things about Dr. Patel. I really can't. I'm very fortunate that all three of my WakeMed doctors in primary care, cardiology and now Dr. Patel, in electrophysiology, are fantastic. They look me in the eyes when we are talking. They listen to me. They take an interest in what I'm saying or what I'm going through. They each genuinely take good care of me. I recall one time I was hospitalized for fluid on my lungs. Dr. Godiwala stopped in to visit me every day on his way to his clinical practice. Dr. Patel called and checked on me. This level of care is something a patient will never forget."
About WakeMed Heart & Vascular
WakeMed Heart & Vascular physicians bring together expert cardiologists along with cardiovascular, thoracic and vascular surgeons who are dedicated to delivering the highest level of cardiovascular care in Raleigh, Apex, Benson, Cary, Dunn, Fuquay-Varina, Garner, Morrisville, Wake Forest and Clayton, N.C. For decades, these physicians have chosen to bring their talent and expertise to WakeMed for its reputation for excellence in cardiovascular care and commitment to providing the most exceptional patient experience.
Pulmonary Rehab and Cardiopulmonary Therapy
The goal of cardiopulmonary therapy is to help participants be more independent and active without getting short of breath. Many participants enjoy losing a little weight too! WakeMed Cardiopulmonary Therapy includes:
- Closely monitored exercise
- Breathing exercises & strategies
- Nutritional information
- Tips on saving your energy to do the things you want to do
- Educational sessions to help you understand and manage your health
The group meets five days a week for four weeks — three hours a day. The program is led by a specially trained physical therapist and a team of respiratory therapists and clinical aides. They will design a plan that meets your specific abilities and goals.