Getting to the Root of Sleep Problems
October 30, 2025
By: WakeMed Health & Hospitals
Categories: Sleep Medicine, Cary Hospital
Tags: Sleep Medicine, Sleep Apnea, obstructive sleep apnea, narcolepsy, spring forward, fall back
Good sleep is critical to your long-term health. In fact, not getting the sleep you need can increase your risk for a whole host of health problems, including obesity, heart or kidney disease, high blood pressure, diabetes and stroke. Sleep is also important for your mental health and sleep deficiency has been linked to depression, suicide and risk-taking behavior. Children can have sleep problems as well.
WakeMed Sleep Medicine specialist Cameron Barber, DO, explains, "When a child has obstructive sleep apnea, oftentimes the first symptoms are bedwetting in a six- or seven-year-old child after being dry for years, or a preteen might suddenly present with symptoms of attention deficit hyperactivity disorder (ADHD). This happens because their bodies are struggling with sleep deprivation."
So, how do you know in adulthood if you have a sleep problem? While you may have a poor night of sleep or feel tired now and then, common signs of a true sleep disorder include these:
- You don’t feel refreshed in the morning.
- You take regular naps — or feel like you need one most days.
- You fall asleep at inappropriate times or feel excessively sleepy during the day.
- You snore when you sleep.
- You have high blood pressure and/or atrial fibrillation.
Diagnosing Sleep Problems — Do You Need a Sleep Study?
If you’re concerned about your ability to sleep, it might be time for a sleep study. Sleep studies are used to diagnose common sleep disorders, such as obstructive sleep apnea, rapid eye movement (REM) behavior disorder and periodic limb disorder, among others.
Sleep studies can be performed at home or in a sleep study facility. The initial sleep study is often conducted at home.
Dr. Barber shares, "A home sleep study is a screening tool to look for obstructive sleep apnea. The premise of a home sleep study is that we can get an idea of what is happening with you in your natural sleep environment. It involves clipping a small black box on your night shirt with a chest belt, a belly belt, a nasal cania for airflow and a little finger and wristwatch for oxygen and heart rate monitoring. Throughout the night, your airflow is tracked to see if it diminishes and to see if you have a weak or stopped breath."
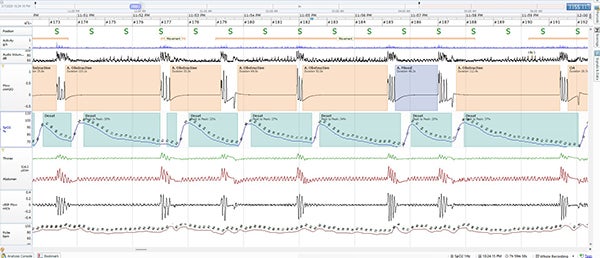
An in-lab sleep study, also known as polysomnography, is a non-invasive diagnostic tool that allows your doctors to monitor your brain and body while you sleep. An electroencephalography (EEG) monitors your sleep stages and how much time you’re in REM vs nonREM sleep. An electomyography (EMG) keeps tabs on your muscle function while you sleep. Sensors for the airflow, blood oxygen level and respiratory movements will show if you stop breathing during sleep. Together, they’ll give your doctor a clearer picture of your sleep patterns, which can help diagnose common sleep disorders.

Dr. Barber adds, "In an in-lab sleep study, we attach wires on your head along with the chest and belly belt, to monitor your brain waves, chin leads, muscle activation in your legs, heart rate and oxygen. One of the best things about our WakeMed Sleep Center is our use of Bluetooth, so you are wired up, but you're self-contained and not tethered to a monitor. If you need to go to the bathroom, you just get up and walk to the bathroom. You don't have to wait for a sleep tech to come in and disconnect you."
WakeMed’s Sleep Center & What to Expect
Our state-of-the-art Sleep Center in the Health Park at Kildaire facility in Cary is near WakeMed Cary Hospital. The sleep lab rooms are just like normal hotel rooms — you’ll have a private bedroom and bathroom, and you’re welcome to bring personal items, such as your favorite pillow or blanket. In most cases, you’ll arrive around 8 pm and a professional sleep technologist will place sensors on your body to monitor your sleep overnight. Then, you can either read or watch TV until you’re ready to go to sleep. Patients leave around 6 am.
Some in-lab studies occur during the day, so you can learn how to use the machine. Narcolepsy testing is done as a day-time nap. Patients are given five nap opportunities at 8 am, 10 am, 12 pm, 2 pm, and 4 pm. If you can fall asleep in fewer than eight minutes, it could indicate narcolepsy.
During your in-lab sleep study, our team will use the latest technology to monitor your brain waves, muscle activity, leg movements, heart rhythms and other body functions. Testing is completely painless. Data from your test is collected, scored and interpreted by a sleep specialist, and sent to your referring physician for recommended treatment.
Featuring a calming and comforting atmosphere, convenient parking and state-of-the-art diagnostic testing, our Sleep Center boasts these features:
- Sophisticated décor with queen-size beds.
- Private restrooms (with walk-in shower) and control over room temperature.
- Flat screen, high-definition televisions featuring Spectrum cable in each room.
- Continental breakfast in the morning.
Treatment Options
If you are diagnosed with sleep apnea, you will likely receive a continuous positive airway pressure (CPAP) machine. These machines are non-invasive and portable. The machine's sound is now a whisper compared to older models. The CPAP machine monitors your breathing, and when it sees an obstruction, it goes up in air pressure, giving you enough pressure to keep you asleep.

Dr. Barber notes, "Other types of CPAP machines are available, called bi-level PAP, adaptive servo ventilation (ASV), volume-assured pressure support (VAPS). If you find that CPAP is not for you, we have other options to help you sleep. Options include oral appliances; Inspire™, which is a nerve stimulator for the nerve of the tongue; and even jaw surgery."
The Impact of Falling Back and Springing Forward on Sleep
Not only can sleep apnea impact sleep, the ritual of day light savings time also impacts sleep with negative consequences.
Adjusting the clocks back to end daylight saving time can significantly affect your sleep patterns. When you gain an extra hour, it might seem like a bonus, but it can disrupt your internal body clock or circadian rhythm. You may find yourself feeling groggy or out of sync as your sleep schedule shifts. This change can lead to difficulties in falling asleep or waking up, as your body takes time to adapt to the new routine. Ultimately, while the extra hour might be nice, it can create a ripple effect on your overall sleep quality.
Dr. Barber says, "The best way to prepare is to keep the current schedule and not go to bed an hour later. If you need to adjust to the new time, adjust your sleep schedule by 15 minutes over four days leading up to the end of daylight savings time, so your body is not so shocked by the impact."
Daylight saving time can also confuse your sleep schedule as you "spring forward" an hour. This shift often leads to disrupted sleep patterns, making it harder to fall asleep and wake up feeling refreshed. The sudden change can affect your internal clock, resulting in grogginess and decreased alertness in the days following the transition. Adjusting to the new time can take a toll on your overall well-being, highlighting the importance of gradually adapting your sleep routines to minimize the impact.
Dr. Barber is not in favor of daylight savings time, but he urges people to take steps to preserve their circadian rhythm as it approaches.
"That's when prepping yourself in advance is more important to minimize the effect of losing the hour of sleep. You go to bed about 15 minutes early for a few days, whether or not you are a morning lark or night owl. Your body aligns that circadian rhythm very strongly to the sun. And when the sun is directly at noon overhead, our bodies know that. That and when we've mismatched it by a full hour for daylight savings time, will we get more time at night? Well, now people who are going to bed later are going to bed even later and they can't wake up artificially early for their jobs and we just end up with chronic sleep deprivation."
To schedule an appointment for a sleep study at WakeMed Cary Hospital Sleep Center, please call: 919-782-7240