Prostate Cancer and Treatment
As the second most common cancer among men (behind skin cancer), prostate cancer is likely to impact one in nine men during their lifetime. With more than 3 million cases in the US and nearly 200,000 new diagnoses made each year — early detection can help save lives. While many men live for years without knowing they have prostate cancer, it can spread. Urologists take many approaches to treatment, including watchful waiting and other medical interventions. In some cases, urologists may recommend removal of the prostate.
That’s why WakeMed Urology encourages screening for prostate cancer early and often — in compliance with national guidelines as set forth by the American Urological Association (AUA).
Common Symptoms of Prostate Cancer
Prostate cancer is silent in the initial stages, but later on, these symptoms may occur:
- Frequent urination, especially at night
- Difficulty in starting or stopping urination
- Weak or interrupted urine flow
- Painful and/or burning when urinating; blood sometimes in urine
- Pain with ejaculation and sometimes blood in semen
- Discomfort or pain in lower back, hips and legs
Prostate Cancer
As mentioned, a prostate cancer diagnosis doesn’t always result in treatment. Sometimes “watchful waiting” is advised. Other times, medical treatment – biopsy, resection or radiation therapy – is recommended.
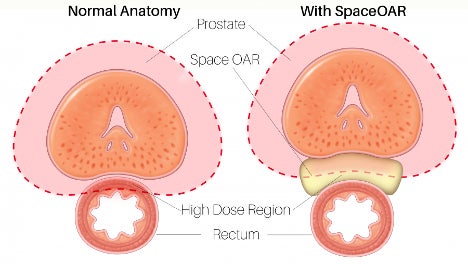
Patients that opt to treat their prostate cancer with radiation can often face potential side effects because of the proximity of the rectum and the prostate. These unintended damages can include fecal incontinence issues or other longer lasting side effects.
WakeMed Urology offers a minimally invasive procedure which inserts a temporary spacer between the rectum and prostate to protect the rectum from damage during radiation therapy. This can help maintain the function of the rectum for the patient. Learn more about the SpaceOAR Hydrogel procedure.
Prostate Cancer Treatment
If you’re diagnosed with prostate cancer, you can expect exceptional, compassionate care from our multidisciplinary team of urologists, medical oncologists and radiation oncologists. Learn more about the WakeMed Cancer Care team.
Treatment options may include radiation, chemotherapy, immunotherapy, or other new emerging treatments — all of which would be recommended and/or administered by an oncologist. If your cancer hasn’t spread and you’re otherwise healthy, a surgery (prostatectomy) to remove your prostate gland and/or surrounding tissue may be an option.
WakeMed Urology has decades of expertise in performing prostate cancer surgery using the most advanced surgical techniques and/or robotic technology.
Prostate cancer screening and treatment options with Dr. Vijay Chaudhary, WakeMed Cancer Care
Robot-Assisted Radical Prostatectomy
At WakeMed, our fellowship-trained urologists perform robot-assisted radical prostatectomy, which involves the surgical removal of the entire prostate and seminal vesicles. This is recommended typically when the disease is confined to the prostate, with the intent of curing the disease.
Robotic prostatectomy outcomes are comparable to open surgery in terms of both tumor removal and minimizing the likelihood of post-operative side effects, including impotence or incontinence. The technology allows improved vision and dexterity for the surgeon, and reduces blood loss and decreases recovery time for the patient.
After the patent is anesthetized, five small incisions are made across the abdomen and ports are placed in them, four for the robot’s camera and instrument arms and a fifth for passing needles in and out during surgery. An additional, smaller incision is made for the passing of instruments. The urologist is able to reach the prostate precisely by entering the abdominal cavity. The prostate is removed through an incision with a scalpel or similar instrument. In most cases, the lymph nodes are then removed for sampling to guide future treatment. Robotics allows the intricate dissection of the lymph nodes from nerves and blood vessels with minimal blood loss and accuracy. Once the tissue has been removed, the area is cleaned with sterile solution, a catheter is inserted and the incisions are closed.
In general, robot-assisted prostatectomy requires a one- to two-day hospital stay. The day after surgery, patients are encouraged to walk. The catheter will be removed in about one to two weeks, based on how the connection between the bladder and urethra have healed. Most patients can return to normal activities within a month following surgery; however, urinary and sexual function may take a few months to a year to improve.