.
What is Pilonidal Disease?
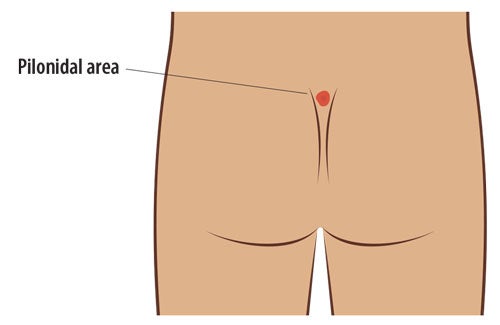
Pilonidal disease (which includes pilonidal “cyst," pilonidal abscess, and pilonidal sinus) is a chronic skin and subcutaneous fat infection in the crease of the buttocks. This typically occurs in patients aged 12–26 years of age. The condition is usually the result of hairs that become trapped beneath the skin in the gluteal cleft (crease between the buttocks) and become infected or trigger a chronic inflammatory reaction in the adjacent tissue.
Many patients that have pilonidal disease experience uncomfortable, raised areas with small openings draining clear, cloudy or bloody discharge. Redness, swelling, pain with sitting and severe tenderness are indications of possible acute abscess formation.
While pilonidal disease is very common in adolescents, many primary care physicians are unfamiliar with its cause and the best treatment practices. Patients may suffer for months or even years prior to diagnosis. Unfortunately, pilonidal disease has a very high recurrence rate if not treated properly.
Our pediatric surgeons offer a variety of treatment options, including the minimally invasive Gips procedure (also called “trephination” or “pit picking”) as well as excision with flap coverage for more extensive disease. We are experienced in the use of the cleft lift advancement (Bascom) flap and the rhomboid (Limberg) flap for these more complex patients.
Read more about what to expect before and after pilonidal disease surgery in our patient handbook.
Treatment: Trephination (Gips Procedure)
The trephination procedure, also known as “pit picking,” was originally developed in the 1990’s in Israel, then reported in the surgical literature in 2008. This procedure involves removing pilonidal sinus tracts with “trephines,” which are small scalpels with circular blades that are typically used for skin punch biopsies. The small openings created by circular blades allow the surgeon to access the underlying cavity and remove the trapped hairs and chronic inflammatory tissue contained within that space. This procedure has gained worldwide acceptance and is now considered the treatment of choice for mild pilonidal disease. This can be performed under conscious sedation with local anesthetic in our pediatric outpatient minor procedure suite (POMPS) or under a brief general anesthetic in the operating room. This is an outpatient procedure, without overnight hospitalization. During the procedure, packing material (a long skinny gauze) is placed in each opening, then gradually removed over the course of four to five days. The risks of trephination are minimal, limited to bleeding, small chronic open wound, and recurrent pilonidal disease, which ranges from 5% at one year to 20% or more at 10 years.
Benefits of trephination:
- No activity restrictions after procedure
- Early return to school or work
- Minimal pain after procedure
Cleft Lift Procedure (Bascom Flap):
The cleft lift procedure is designed to manage moderate to severe pilonidal disease, usually characterized by multiple chronic open wounds and extensive sinuses. This procedure involves excision of the entirety of the disease with an asymmetric incision with a goal of elevating the cleft and moving it a bit off of midline to prevent recurrent disease. This procedure does require a drain to be placed at the time of surgery, which usually stays in place for three to four days but sometimes needs to be left in longer due to high output. The cleft lift procedure is associated with activity restrictions following surgery, especially with respect to deep squatting and contact sports. The risks of the cleft lift procedure include recurrent pilonidal disease (up to 5% of cases), wound infection, hematoma, seroma formation, and wound separation (up to 10% of cases).
Benefits of cleft lift:
- Closed wound with no packing
- Lowest recurrence rate of all flap procedures
Post-Operative Care
Reports rates of recurrence following surgery for pilonidal disease vary widely. It is our belief that meticulous hair removal from the buttocks and gluteal cleft and meticulous wound care are essential for success. We therefore strongly recommend frequent follow-up office visits to ensure that your child achieves complete healing. These visits are typically once a week for the first two to three weeks, then spaced out a bit (every few weeks), depending on the patient and progression of healing.
Hair management is a crucial part of treating pilonidal disease, especially in our most hirsute patients. Use of clippers and depilatory cream are helpful but require routine use to be effective. Attempts to use intense pulsed light (IPL) machines for non-operative management of pilonidal disease have not been successful. However, post-operative use of IPL has been shown in multiple well-designed studies to significantly reduce the risk of recurrent disease. Unfortunately, the laser technicians at most centers fail to adequately treat skin areas deep within the gluteal cleft.
To address this issue, our pediatric surgery team has established a collaboration with Dr. Scott Hultman, head of the plastic and reconstructive surgery team at WakeMed. Dr. Hultman and his team use IPL to intentionally damage hair follicles and inhibit future hair growth within the buttock crease. This is initiated after complete healing from pilonidal surgery and typically performed every four weeks using topical anesthetic gel or cream. Some health insurance providers have recognized the dramatic overall cost savings with this approach and are now considering laser hair removal a “covered service.” For those who do not have insurance coverage, a discount is available to families who choose to pay with cash.