Illustrating in Technicolor: Hide Terada's Post-Concussion Syndrome Story
March 26, 2024
By: WakeMed Health & Hospitals
Categories: Emergency, Primary Care, Stories, Physical Therapy
Tags: Trauma, Concussion, post-concussion syndrome, brain injury
Hide Terada has always been the life of the party. With his incredible sense of humor, genuine interests in others and fun-seeking personality, he's consistently found joy in life circumstances. Then, an event occurred in 2019 that would test his resolve and outlook, inspiring him to illustrate the life he could aspire to — even if in technicolor.
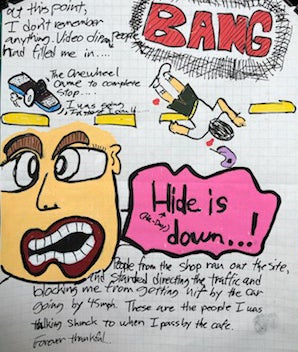
On Sunday, July 14, 2019, Hide was taking a break during his shift as a barista. To have a little fun, he decided to go for a short spin on his one-wheel electric skateboard.
Speeding to upwards of 30 miles per hour along the strip, he relished these fleeting free moments, the wind rushing through his helmet.
"I was peeling out and yelled to passersby, "Who needs two wheels? I have one wheel!"

Fun Comes Crashing to a Halt
Almost immediately the board screeched forward as Hide lost his balance and went flying through the air, whirling into oncoming traffic near the downtown Raleigh Capital Boulevard intersection. He slammed to a stop, banging his head on hot asphalt.
Cars converged around Hide to shelter him from being hit by motorists. Others on foot ran to the scene, including Hide's friend who worked in the café. Hide moaned, writhing in pain from the hit.
A friend called Carissa, Hide's wife. He informed her of the accident and asked permission to call 911 and have him transported to WakeMed Raleigh Campus Emergency Department as a trauma alert patient. She consented and told him that she'd meet them at the hospital.
Before long, an ambulance arrived, and Hide was loaded onto a stretcher and taken to WakeMed.
A Diagnosis at WakeMed
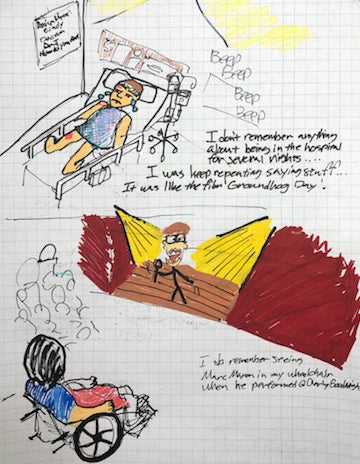
When Carissa saw her husband, he was in a hospital bed covered in lacerations and intermittently calling out coffee orders while complaining that he urgently needed to return to work. Hide was confused and overwhelmed. The care team took him to Imaging Services and diagnosed him with a moderate concussion and two mild fractures along his shoulder and hip. He also had road burn and lacerations to various parts of his body.
Hide was then transported to another hospital system where his insurance was preferred. He remained their for two days and was discharged home. He continued with outpatient physical and speech therapy for about a month and a half.
In time, Hide was feeling better and returned to work.
Symptoms Come Whirring Back
Then, in February 2021, Hide was driving at night for the first time since his accident when he began to feel extremely unwell. He had sudden ringing in his ear, dizziness, extreme sensitivity to light and mental confusion. He felt desperate to get home. When he finally arrived, he realized his balance was off, and he was having trouble tracking movement with his eyes.
"I remember when I got home I had to go into a dark room and bring myself down. It was a resetting period. That was the beginning of my relapse as sensitivity to light and over stimulation with busy environments returned. It was over sensory cascading into my brain."
Discouraged but hopeful, Hide and his wife, Carissa, made the difficult decision that he should quit his job and take time to rest and recover. By late fall, he was still functioning at the lowest level, so Hide called his primary care provider, Dominick Trapani, DO.
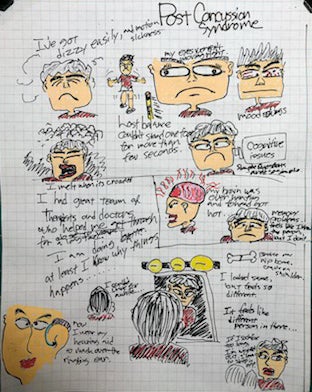
 Dr. Trapani assisted Hide in restarting physical therapy and, along with therapist Amanda Cole, helped Hide connect with concussion services available through WakeMed. On December 30, 2021, Hide received a comprehensive neurological specialist exam and was diagnosed with post-concussion syndrome.
Dr. Trapani assisted Hide in restarting physical therapy and, along with therapist Amanda Cole, helped Hide connect with concussion services available through WakeMed. On December 30, 2021, Hide received a comprehensive neurological specialist exam and was diagnosed with post-concussion syndrome.
"I am fortunate to serve as Hide's primary care physician and with his trust I was able to help guide him after his accident to my wonderful WakeMed colleagues. Hide has made great progress with his post-concussion rehabilitation with his hard work assisted by the WakeMed team. Hide 2.0 should serve as an inspiration to others who suffer a traumatic head injury that sometimes we have to pivot in life but that is just part of the journey."
Post-Concussion Syndrome
Post-concussion syndrome happens when symptoms of a brain injury last longer than expected (more than three months). Common symptoms may include the following:
- Cognitive issues (thinking, remembering)
- Dizziness
- Fatigue
- Headache
- Irritability
- Mood changes
- Sleep disturbances
"By this time I was in a desperately low state. I'd been struggling for months, delaying care. I'd spent months unable to drive, go to the grocery store or carry on conversation for more than four minutes without a flare up. Flare ups involved feeling off balance, difficulty thinking, trouble with eye-tracking, extreme sensitivity to any stimuli and generally feeling unwell."

 Hide received care through August 8, 2022.
Hide received care through August 8, 2022.
Amy Schultz, MS, OTR/L, ATP/SMS, CLT, provided occupational therapy (OT), helping him retrain his brain and body to optimally engage in the environment around him. OT assisted with optimizing his ability to use his visual system to take in the environment around him, as well as to improve his ability to multitask. Over time, Hide was able to also incorporate energy conservation and body scanning principles to increase his tolerance for higher stimulation environments allowing him to improve his environmental tolerance should he return to work as a barista.
Cognitive-communication skill and strategy training were provided by Amanda Cole, MS, CCC-SLP.

Cole explains, "Hide's speech therapy focused on collaborative goal setting with applying compensatory strategies (such as energy conservation and executive functioning techniques) to help him get back to his preferred activities."

Chelsey Freed, PT, DPT, provided physical therapy.
"My involvement in treating Hide was for physical therapy for chronic back pain that developed as a result of his injuries following his accident. Our focus was on core strengthening for spinal stabilization, posture re-education, lifting mechanics, diaphragmatic breathing and home exercise program development. Over time, Hide learned how to better manage and cope with his chronic back pain by learning new strategies and understanding how to be in control of it all. Our motto throughout therapy was 'crushing it.'"
 Freddie Rivera, MA, LCMHC, NCC, provided talk therapy using therapeutic approaches, such as cognitive-behavioral therapy and person-centered therapy, to provide Hide the support he needed to develop coping skills, achieve personal goals, and find acceptance in his life, through WakeMed Mental Health & Well-Being Virtual Behavioral Health services.
Freddie Rivera, MA, LCMHC, NCC, provided talk therapy using therapeutic approaches, such as cognitive-behavioral therapy and person-centered therapy, to provide Hide the support he needed to develop coping skills, achieve personal goals, and find acceptance in his life, through WakeMed Mental Health & Well-Being Virtual Behavioral Health services.
Rivera says, "It was a pleasure working with Hide in his journey to reinvent himself while finding happiness again in his life."
"They each did a lot to help me. Occupational therapy helped me start rethinking my career path. Physical therapy addressed pain I was having, particularly in my back. Speech therapy was much more than speech. Amanda really helped me a lot with cognition. Physical therapy meant a great deal throughout the entire process. I appreciate Chelsey. And, Freddie held my hand virtually, walking me through my tough time. I've always been a happy guy, but the accident changed me. Hide 2.0 is not the same guy. I had to accept that."
Together, Hide and his wife, Carissa, accepted that life had changed, and they must forge a new path forward.
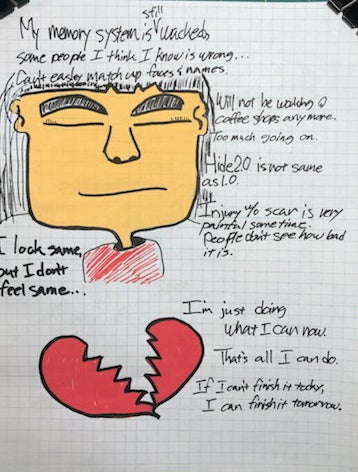
"I used to love a lot of stimulation, but now I need more quiet. My hope is to one day be a professional illustrator. I'm grateful for my wife, my life partner, because she accepts that our lives will look different now, and all she wants for me is that I do what makes me happy."
Gratitude for WakeMed

"Now, I am walking this new journey as Hide 2.0. WakeMed care teams taught me how to deal with my daily problems. Those tools are my treasure. I still have problems with facial recognition and names. I also can't handle long, detailed conversation; impromptu decision-making; and crowded places, but I've got a purpose in my life. I want others to see that life after head trauma can be a life worth living. I'm grateful that WakeMed helped me see that."
About WakeMed Brain & Spine
Our distinction in cardiac and vascular procedures extends to brain and spine health with specialists in cardiovascular and neurovascular intervention working together to manage complex central nervous system vascular disorders.
A center of excellence, you can be certain of our superior value. We deliver comprehensive diagnostic and treatment plans with exceptional outcomes, individualized to the needs of each patient.
We offer numerous services, such as neurodiagnostics, to treat an array of conditions affecting the brain, nerves and spine.
About WakeMed Mental Health & Well-Being
When an emergency related to a new or existing mental health issue arises, mental health crisis services can often provide more appropriate care than emergency rooms. Services are available to adults and children who need immediate help with addressing mental health and substance use issues, It can also help those who need short-term supportive therapy to help manage their mental health and improve their overall wellness.
About WakeMed Outpatient Neuro Rehabilitation
At WakeMed Outpatient Neuro Rehabilitation, our physical therapists, occupational therapists, and speech therapists excel in evaluating and treating adults and older children after stroke, spinal cord injury, traumatic brain injury, concussion, and other neurological conditions. Our practices in Raleigh, Cary, and Clayton are staffed by specialty trained, passionate therapists who work one-on-one with clients to help them achieve their goals.
About WakeMed Physical Therapy
It’s our goal at WakeMed Physician Practices – Physical Therapy to get you back to your active lifestyle. Our techniques are based on national best practices to ensure you receive the latest, best treatment for your condition. We provide physical therapy and occupational therapy in Raleigh, Cary, the Brier Creek area and Apex, North Carolina.
About WakeMed Raleigh Campus Emergency Department
As part of the Raymond L. Champ Centers for Emergency Medicine on our Raleigh Campus, the adult emergency department is available around the clock, 365 days a year to treat everything from minor cuts and broken arms to something more serious like stroke, a heart attack or major trauma.
The Adult Emergency Department on the WakeMed Raleigh Campus is home to Wake County's only Level I Trauma Center, as well as a nationally accredited Chest Pain and Primary Stroke Center. Raleigh Campus adult emergency department is one of the busiest emergency departments in the state.