Atrial Fibrillation
Atrial fibrillation, or“AFib,” is the most common heart rhythm disorder (cardiac arrhythmia), it is the cause of 15 percent of preventable strokes among Americans and approximately 2 million Americans have it. It is an irregular, rapid and quivering heartbeat.
Although AFib tends to progressively worsen in most people, it is treatable, particularly when patients seek help early — when they first begin having symptoms or when their doctor first suspects it.
Understanding the basics of atrial fibrillation is the first step in preventing its harmful complications, including stroke and heart failure.
About Atrial Fibrillation
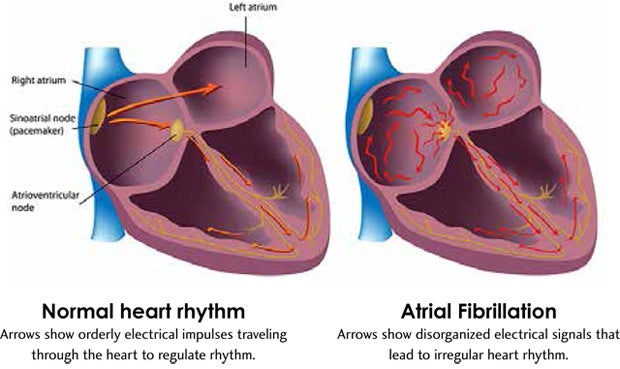
When the heart beats regularly, its two upper chambers (atria) are beating in sync with the heart’s two lower chambers (ventricles).
The left atrial appendage is a small pouch located in the left atrium. As the heart beats, blood from the left atrium and left atrial appendage is pushed into the left ventricle. In atrial fibrillation, the atria do not have sufficient time to contract and move the blood to the ventricles. The atria quiver and the heartbeat becomes rapid and erratic.
This creates areas of slow blood flow that are predisposed to blood clot formation. If a blood clot breaks free and lodges in an artery leading to the brain, a stroke occurs. Blood thinners, when appropriate, can dramatically reduce the risk of stroke.
Causes of Atrial Fibrillation
Aging is a risk factor for AFib, with people ages 65 and older more likely to develop the condition than younger individuals. Other risk factors include:
- Heart failure
- Diabetes
- High blood pressure
- Sleep apnea
- Family history of atrial fibrillation
- Alcohol and stimulants
- Coronary artery disease, which is the narrowing of arteries that supply blood to the heart
- Thyroid disorder
- Obesity
Symptoms of Atrial Fibrillation
Although some people with AFib experience no symptoms, the condition commonly causes symptoms that include:
- Heart palpitations, which can be steady or intermittent, that come from erratic and irregular ventricular contractions
- Shortness of breath
- Fatigue
- Feeling of weakness
People with AFib who don’t have symptoms are still at risk for stroke. This is one more reason why people of all ages—particularly those 65 and older — should see their doctors at least once a year.
Contact your doctor if you experience any symptoms of atrial fibrillation.
Diagnosing Atrial Fibrillation
The sooner atrial fibrillation is diagnosed, the more effective treatment is. WakeMed’s electrophysiology labs offer the most advanced diagnostic and therapeutic procedures for the evaluation and treatment of AFib. Generally, our cardiologists start with an electrophysiology study, which tests the electrical conduction system of the heart to assess its activity and pathways.
Other techniques we use include:
- Electrocardiography (EKG or ECG): This painless non-invasive testing records the heart’s electrical activity.
- Echocardiogram ("echo") tests: Echocardiography is a type of cardiac imaging that uses sound waves to create moving pictures of the heart and its blood vessels at rest and during exercise. Echocardiogram images help cardiologists diagnose, evaluate and monitor many heart conditions. Types of echo tests include:
- Transthoracic 2-D echocardiography (TTE): This common, non-invasive echo study is performed externally, outside of the chest. TTE can be performed using bubbles (to identify problems with cardiac blood flow) or DEFINITY® contrast (to further clarify imaging).
- Transesophageal echocardiography (TEE): This minimally invasive study can help cardiologists get a closer look at cardiovascular structures if more information is needed after a TTE study.
- Cardiac CT and MRI: Cardiac computed tomography (CT) and magnetic resonance imaging (MRI) are two advanced, non-invasive ways to look inside the heart and thoroughly assess the cardiovascular structures. These can be performed with or without calcium scoring.
Treating Atrial Fibrillation
If AFib is confirmed, treatment depends upon:
- The cause of the AFib
- How long the patient is believed to have had atrial fibrillation
- How burdensome the symptoms are
The top priorities for treating AFib are restoring a normal heart rhythm and preventing blood clots that can cause a stroke. The goal is to return AFib patients to active, happy lifestyles, which is very achievable for most people.
There are many treatments for atrial fibrillation, so if patients don’t respond to one treatment, doctors can try another. AFib treatments include:
Antiarrhythmic medication: Antiarrhythmic drugs reduce the number and duration of AFib episodes by affecting the ion channels of heart cells. In some cases, patients begin treatment with these medications in the doctor’s office. In other cases, patients are admitted to the hospital to receive antiarrhythmic drugs orally or intravenously. The patient’s heart rate is continuously monitored and his or her dosage is adjusted accordingly.
Blood-thinning medication: Many patients are able to prevent clots by taking blood-thinning medications such as warfarin, heparin, rivaroxaban, dabigatran and apixaban. Some patients cannot tolerate these due to increased risk of bleeding and other health complications.
External cardioversion: This delivers an electrical impulse to the heart through paddles or patches placed on the chest. The shock stops the disorganized electrical activity of AFib, resetting the heart into a normal rhythm. Sedation is used so the patient is comfortable. In some cases, transesophageal echocardiography (TEE) is used before an external cardioversion procedure to determine if there are any blood clots in the heart. Patients must take blood-thinning medications before and after to prevent blood clots.
Radiofrequency catheter ablation: Once a patient is sedated, the doctor threads a catheter up to the heart from intravenous access in the patient’s groin—and then isolates the sources of abnormal electrical signals, which are usually located in pulmonary veins. Afterwards, many patients are able to discontinue or reduce the use of antiarrhythmic medications.
Automatic implantable cardioverter defibrillator (AICD): This is a small device that helps the heart beat regularly. Implanted in the chest near the heart, an AICD is equipped with electrodes that sense the heartbeat. It also has a generator that functions as both a heart regulator – shocking the heart to restore a natural rhythm – and a pacemaker, which helps “pace” the heartbeats to keep them from becoming too fast or too slow.
Under general anesthesia, the cardiologist makes a small incision in the upper chest near the collarbone. A wire is run through a vein into the heart and a small cavity is created to place the AICD, which is connected to the wire. While the patient is still under sedation, the unit is tested to ensure the appropriate shock. The procedure takes one to two hours, and most patients remain in the hospital for up to four days for observation.
LARIAT® left atrial appendage closure: WakeMed offers the LARIAT left atrial appendage closure procedure to AFib patients who are unable to take blood thinners. This minimally invasive procedure decreases stroke risk because it allows the cardiologist to seal off the area in the left atrial appendage where many stroke-causing clots tend to form.
While under general anesthesia, the cardiologist makes two tiny incisions — one in the groin and one near the heart. A catheter inserted into the groin is advanced to the left atrial appendage. A guide wire is inserted at the site of the second incision near the heart. Using the two wires, a LARIAT suture-delivery device is used to loop around the appendage and tie it off. This completely seals and stabilizes the appendage, preventing clots from escaping.
After the procedure, patients spend a day or two in the hospital to make sure that the seal remains secure. Recovery is quick, and patients can return to normal activities within a week.
Convergent procedure: A convergent procedure can work for AFib patients with intermittent arrhythmia and structurally normal hearts but for whom medication has not been effective. This treatment involves both an electrophysiologist and a cardiothoracic surgeon.
Temporary transvenous pacemaker: Some AFib patients benefit from a temporary transvenous pacemaker after cardiac surgery, heart attack, infection, medication issues or other concerns. The pacemaker stays in place until the heart rate is stabilized, typically for only a few days.
Make an Appointment
If you or someone you care for is experiencing symptoms of atrial fibrillation, we encourage you to make an appointment with one of WakeMed’s experienced cardiologists. The cardiologist can also refer you to our Atrial Fibrillation Center, where the team can spend dedicated time assessing your symptoms and provide a treatment care plan.
Contact our WakeMed Heart & Vascular – Atrial Fibrillation Center or call 919-350-AFIB (2342)